While medical materials have come a long way toward treating conditions in the body, sometimes they’re a bit too stiff to be a perfect fit. Research at Texas A&M University aims to engineer new biomaterials that will provide effective treatment while also moving better with the body.
“I think at the biggest picture, what gets me excited, is to build dynamic, responsive materials and use those to make medical devices,” said Dr. Taylor Ware, associate professor in the Departments of Biomedical Engineering and Materials Science & Engineering.
Ware’s lab work ranges from new material development to device engineering. One project is finding innovative material solutions to treating urinary incontinence — a condition where there is uncontrolled leakage of urine.
Treatment may include a surgical option where a mesh sling is implanted underneath the urethra to provide support. This device has to balance between ensuring there is no leaking while the person is doing day-to-day activities but can release when they need to void. However, current slings are limited because the clinician has to find the perfect balance to make sure the patient doesn't suffer unintended consequences.
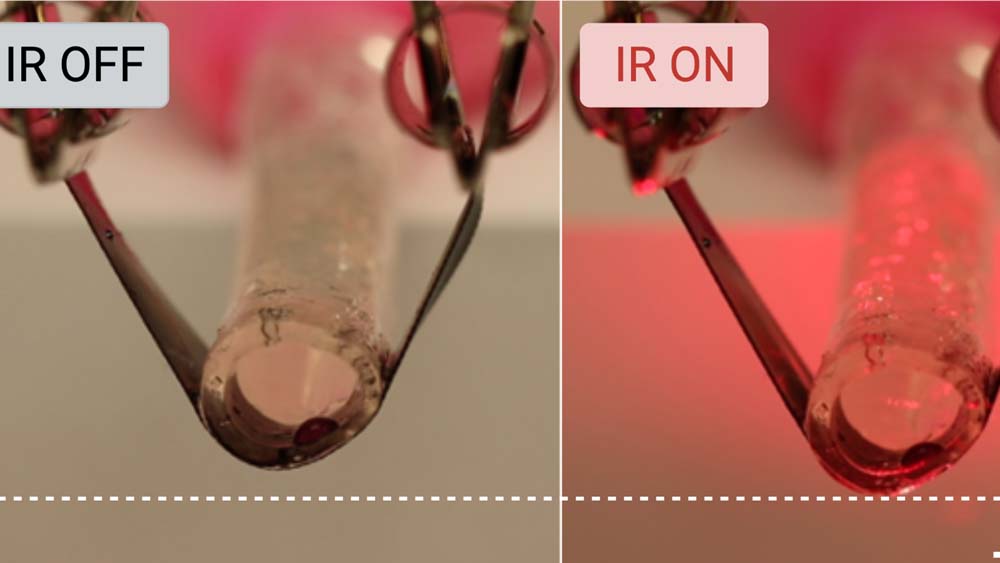
Ware's research aims to develop a device similar to human tissue that’s adaptive, using a type of material called liquid crystal elastomers that react to heat. The team's idea is to 3D print a material that would heat slightly and change shape when illuminated with infrared light, allowing a person to void their bladder easily. When the material cools, it returns to its original shape, allowing the person to remain continent.
In Ware’s lab, this project is led by doctoral student Seelay Tasmim. The work is collaborative with Dr. Philippe Zimmern, professor and clinical urologist at the UT Southwestern Medical Center, and Dr. Mario Romero-Ortega at the University of Houston. The research is funded by the National Institute of Biomedical Imaging and Bioengineering at the National Institutes of Health.
Ware said these types of biomaterials could open the door for a variety of applications.
“These materials are artificial muscles, and we see these materials as useful in a variety of biomedical applications that require mechanical motion,” Ware said. “For example, surgical or even wearable robots may benefit from these soft materials that may be able to replace traditional motors and actuators.”