
Recent discoveries made by researchers at Texas A&M University could change the way ovarian cancer is understood and treated.
Dr. Abhishek Jain, assistant professor in the Department of Biomedical Engineering and the Department of Medical Physiology in the College of Medicine, collaborated with researchers from the Departments of Gynecologic Oncology and Cancer Biology at MD Anderson Cancer Center to gain a better understanding of the interaction among ovarian cancer tumors, blood vessels and platelets. They found that tumors break the blood vessel barriers so that they can communicate with the blood cells, such as platelets. When these tumors come into contact with platelets, they can then metastasize, or begin to spread to other sites in the body.
The collaborative research was recently published in the journal Blood Advances.
Currently, researchers understand that platelets are one of the initiators of ovarian cancer metastasis but did not know what led to the introduction of the platelets to the tumor cells. Instead of struggling to view this relationship in animal models, Jain’s team brought a new solution to the table: organ-on-a-chip research.
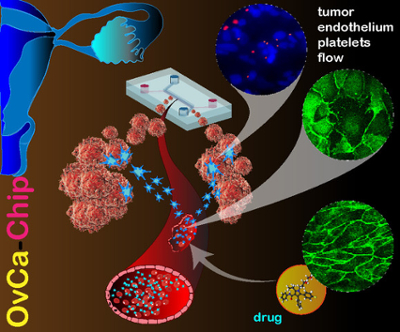
Organs-on-a-chip are microfluidic medical devices the size of a USB drive. The team designed on the OvCa-Chip to give researchers an easier window to view the biological processes between tumors and platelets.
In an interview with the International Society on Thrombosis and Hemostasis, Jain explained that "it basically is a microenvironment where ovarian tumor cells can be co-cultured along with their blood vessels, and then they can interact with blood cells. Once we learn about these interactions, we can then move forward to look into how drugs will impact these kinds of interactions."
Viewing the interaction between tumors and blood vessels on the OvCa-Chip led the researchers to an extraordinary result — the tumor cells systematically broke down the endothelial cells, which are the barrier that lines the interior surface of blood vessels and prevents exterior interaction with blood cells. Once this barrier was gone, blood cells and platelets entered the tumor microenvironment and could be recruited for metastasis.
Harnessing this knowledge could change how clinicians approach ovarian cancer treatment, Jain said, suggesting that anti-vascular drugs could be considered along with anticancer treatments. A benefit of the organ-on-a-chip is that it can also test these novel drug treatments and drug combinations.
Another application of the chips could be diagnostics.
"You have to understand that these are chips that are living. They contain living cells. The advantage is that these are all actually human samples," Jain stated in the interview. "So what we think the future for this technology is, is perhaps we can advance it in the direction of personalized medicine where we could actually take stem cells from patients and other patient-derived cells and make this entire chip from a single patient."