A team of five students in the Department of Biomedical Engineering at Texas A&M University worked over two semesters to find new and adaptable solutions to infant ear deformations — where all the material is there, just not in the right place. As their senior capstone project, the team collaborated with an external sponsor to solve a real-world problem effectively.
“It might, to some people, just be considered a cosmetic procedure, but it actually can cause a huge psychological toll on that child as they're growing up. In severe cases, it can lead to hearing loss,” said team member Ivanna Arizpe. “That's something that we want to limit and resolve the problem before anything can cause them harm.”
The team’s goal was to 3D print a personalized treatment plan to create alternative devices to the generic products on the market, which aren’t exactly fit for infants. Time is of the essence for these devices, as an infant’s ear is only malleable for about the first three months after birth. After that, the problem would likely need plastic surgery to fix.
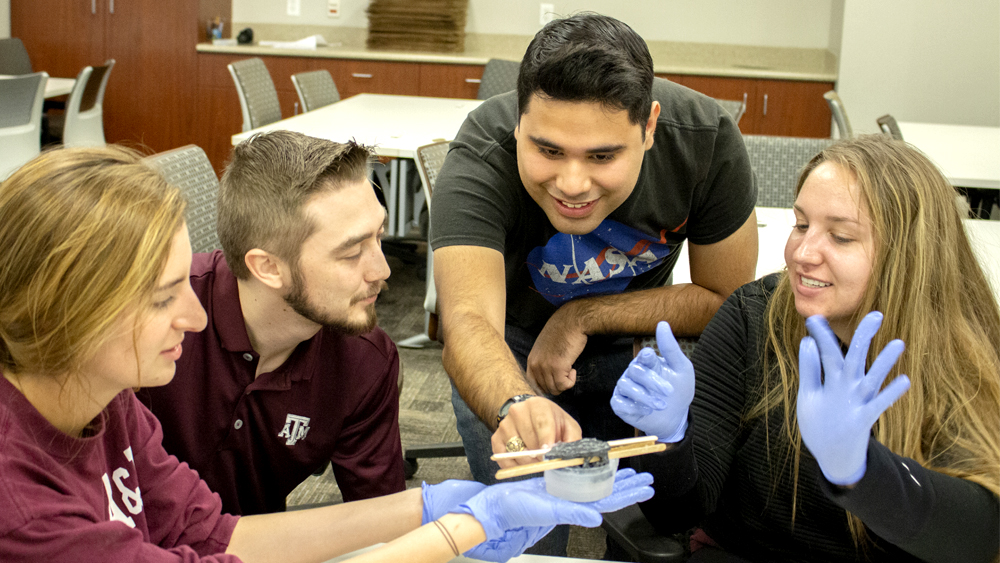
But before they could create the device, the team first had to develop ways to scan, mold and 3D print the ear effectively. The team ran into the challenges, including finding ways to effectively scan an ear and create a process that health professionals will feel comfortable using.
“We need to find a way to make this process easy and manageable for doctors to do so they're not scared to approach this treatment plan,” said Kyle Robinson. “The learning curve is very quick. We’ve really made it a focus because even if we come up with the best device, it's not going to ever be accepted if doctors have no idea how to use it.”
To help address the learning curve, the team developed a standard operating procedure for technicians to enable them to troubleshoot issues.
Along the way, the team also found ways to celebrate their progress. They kept every version of their molds and scans, using a variety of products not formerly designed for medical devices such as fish-tank sealant and modeling clay. Their first successful 3D-printed ear became a sort of mascot the team called Ear-nesto.
Unlike most capstone projects, the team worked with two sponsors from Texas Children’s Hospital, Dr. Sarah Frommer and Dr. Yi-Chun Carol Liu, who submitted similar need statements.

Darby Ballard said interacting and building relationships with both sponsors made a world of difference throughout the project. The sponsors offered their thoughts and opinions but left much of the project’s concept to the students.
“You can never forget that part of engineering is creativity. Being able to take something from concept to prototype and integrating your own twists on that in the way that you want. I think that aspect is something that I was starting to forget prior to this project,” Ballard said. “That’s one of the reasons I wanted to do engineering — because you do get to be imaginative with what you create.”
Having outside sponsors gave the team the chance to travel and meet with an actual patient, even having the opportunity to scan an infant’s ear for reference. Meagan Makarczyk said they received positive reactions from their sponsors and other physicians when they demonstrated their modeling software.
“This is the application of our education, and seeing it and being successful with it helps me know that in the future, wherever, whatever I do with my life, I will be able to achieve something like this because I've already seen results,” Makarczyk said.
Jacob Rodriguez said he could already see how the skills gained from the project can apply to life after graduation.
“Being a part of this project gave me a better idea of what to expect because studying medical devices in class is one thing, but if you have a hands-on experience, you get more of an idea of how to apply your skills in the real world and how to work better with the team,” Rodriguez said. “We’ve gotten to see how a medical device we make can help people live better lives. That’s a pretty rewarding experience.”