
Oral cancer kills more than 10,000 people in the United States every year, even though the survival rate is higher than 85 percent if oral cancer patients are diagnosed early enough. Unfortunately, the majority of patients aren’t diagnosed while the cancer is still in the early stages, something that Dr. Javier Jo is trying to dramatically change with a nearly $1 million, three-year grant from the Cancer Prevention and Research Institute of Texas (CPRIT).
Jo, associate professor in the Department of Biomedical Engineering at Texas A&M University, has been working on this research for more than a decade. The idea came from speaking with oral pathologists about relevant problems in their clinical practice. Dentists and physicians typically rely on the naked eye to look for lesions in a patient’s mouth that may be cancerous and should be further examined with a biopsy, but identifying these areas can be difficult because a patient’s mouth can form lesions that may be benign, precancerous or cancerous.
Jo’s research is seeking ways to improve the number of cancerous lesions caught at the early stage while reducing the number of unnecessary and painful biopsies of benign lesions.
“Even though these lesions are right there and you can see them, only 30 percent of patients are diagnosed at the early stage,” Jo said. “We believe that’s in great part because it’s very difficult to make decisions about what lesions really need to be biopsied since cancerous lesions are not easy to distinguish from benign lesions, even for experienced dentists and oral pathologists.”
Jo’s team has tested several endoscopic imaging technologies to identify potential cancerous oral lesions. The most promising one so far is a fluorescence endoscope that illuminates the lesion with a certain color of light to make the lesion glow, and the glowing or fluorescent lesion is then imaged with the same endoscope. The medical imaging instrument being developed is noninvasive and requires no chemical to be applied to the patient to enhance the image. The team is now fabricating these fluorescence endoscopes to deploy them to different clinics in Texas and start imaging patients with suspicious oral lesions.
“The fluorescence endoscopy data that will be collected will be used to continue developing and validating the numerical methods of the computer-aided diagnosis (CAD) system, which is the software that will allow us to process the fluorescence endoscopy data, and transform it into useful diagnostic information,” Jo said.
The main impact of this technology is that it could lead to a significant increase in the percentage of patients that are being diagnosed at the early stage...
Jo said that the specific goal of the CPRIT grant will be to continue developing the CAD system software that will interpret the fluorescence endoscopic lesion images.
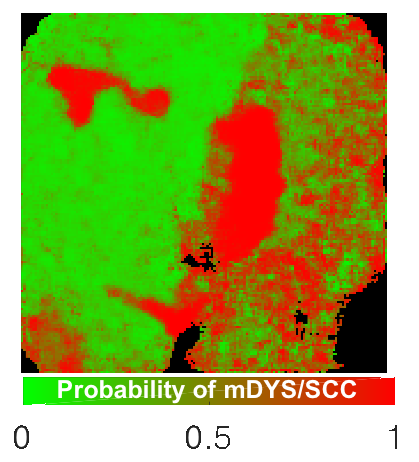
To train the CAD system, Jo’s team will be collecting fluorescence endoscopy images of suspicious oral lesions to build a large database that could be datamined in order to identify characteristics in these images that are specific to premalignant or malignant oral lesions. Once the lesion is scanned, the CAD system will compute and display a color map of the area where certain colors will indicate a high probability of the lesion being benign or cancerous.
“As we continue to collect more images, we will continue to improve the CAD system that hopefully will be able to provide diagnostic information with sufficient accuracy to be useful to help the dentist or oral pathologist to make a sound decision on how to clinically manage a patient presenting a suspicious oral lesion,” Jo said.
Jo said the ultimate goal is to offer the tool to dentist’s offices to assist with the screening of oral cancer, and to oral pathologists to assist with the diagnosis of oral cancer by providing guidance during the biopsy examination.
“When the lesion is really large, the oral pathologist cannot take multiple biopsies and kind of has to guess the best place from where to take the biopsy,” Jo said. “We think that our tool could also provide guidance to the oral pathologist to indicate where the greater chances of cancer are in the lesion so that the biopsy would be taken from that location.”
“The main impact of this technology is that it could lead to a significant increase in the percentage of patients that are being diagnosed at the early stage, that’s our main motivation,” Jo said. “If we can facilitate the identification of oral cancer patients while the cancer is still a small lesion as opposed to when it has already metastasized to other parts of the body that would make a huge clinical impact to oral cancer patients.”
In the last three years Jo’s research program has received close to $4.5 millions of combined international, federal and state research funding toward the development of this transformative clinical imaging technology.
“We strongly believe that our technology could potentially be used to assist at every stage of the clinical management of oral cancer patients, not only for screening and early diagnosis, but also for guiding treatment and monitoring for cancer recurrence,” Jo said.
Jo’s team in this CPRIT grant includes Dr. Yi-Shing Lisa Cheng and Dr. John Wright, professors in the College of Dentistry at Texas A&M; Dr. Nadarajah Vigneswarab, professor in the School of Dentistry at The University of Texas Health Science Center in Houston; Dr. Thomas Schlieve, assistant professor in the Department of Surgery at The University of Texas Southwestern Medical Center; and several postdoctoral fellows and students in Jo’s research lab, including Dr. Rodrigo Cuenca-Martinez, Dr. Jose Rico-Jimenez, Michael Serafino, Elvis Duran-Sierra and Oscar Benavides.