The Kleberg Foundation recently awarded Dr. Gerard Coté, professor in the Department of Biomedical Engineering at Texas A&M University and director of the Center for Remote Health Technologies and Systems, and his multidisciplinary team a $957,789 grant to advance research on user-centered diabetes technology for underserved communities in South Texas.
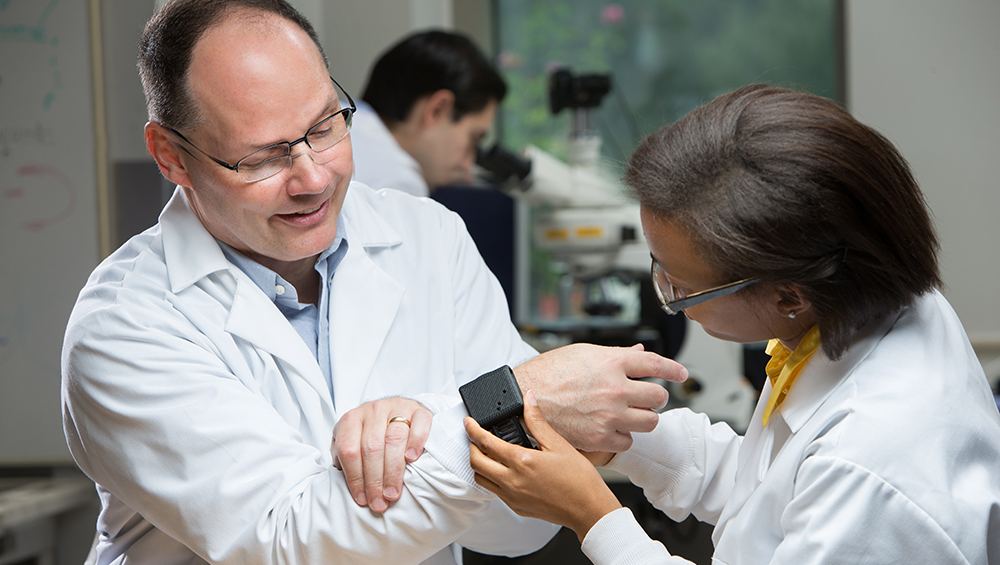
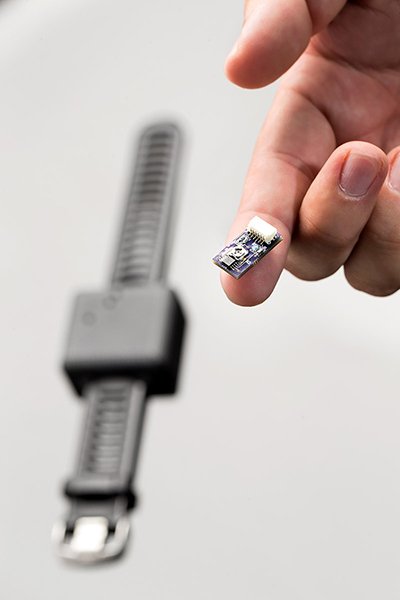
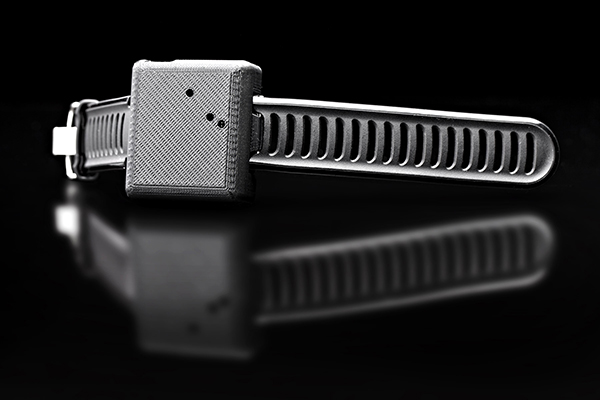
Over the next three years, the research team expects to design a next-generation continuous glucose monitor that is innovative, affordable and accessible. The newly designed monitor is envisioned to be a biocompatible sensor the size of a grain of rice placed inside the body, near the wrist. A new smart wristband will wirelessly transmit glucose measurements to a smartphone app. The app will then send updates to the patient regarding glucose levels and possibly information regarding diet and medication.
Alerts will notify the patient if they need to adjust their insulin levels, take a glucose tablet or seek medical help. If a patient is approaching a glucose crash, which is a possibly life-threatening situation, medical personnel
One of the device’s greatest advantages is that it will work at night. If a patient’s glucose levels are too high or too low, an alarm will sound, relieving the stress of the parent or spouse who often wakes up in the night to check on the patient.
The device will also create individual data trends over time for patients and doctors to assess and make informed future decisions. “Empowering the patient is our number-one priority,” said Coté. “Although the focus of their research is underserved groups in South Texas, the technology will have worldwide implications for improving the lives of people with diabetes.”
Why South Texas?
Many of the communities in South Texas are medically underserved, painting a dire local picture that represents the overall health disparity issue across the United States. The team is filling a research gap by focusing on South Texas, a 27-county region where 20 percent of the population has diabetes and 73 percent are at risk of developing it. The region also has a higher rate of diabetes-related deaths in border counties than all non-border counties combined.
“We must facilitate access to health care for the underserved communities of South Texas,” said Dr. Farzan Sasangohar, one of the project’s co-principal investigators. “Right now, the technology to manage diabetes is not affordable and it’s not
The adoption rate for continuous glucose monitors, the most commonly used insulin tracking technology, is extremely low in South Texas. Although more advanced than the blood glucose test, continuous glucose monitoring is intrusive and expensive, making it out of reach for the underserved. “It’s critical that the technology is
The project is unique in its focus on making the new technology accessible. The industrial and systems engineering contribution to the project includes incorporating user feedback into the design process to make the new technology an easy to use, sustained intervention for patients. Sasangohar is an industrial and systems engineering professor and the director of the Applied Cognitive Ergonomics Laboratory, whose focus is on human interaction with technology. “I strive to understand how humans play a role in human-systems interactions,” said Sasangohar. “Humans are key elements of complex sociotechnical systems but are also sources of uncertainty and large variability.”
The project is a multidisciplinary collaboration that includes six principal investigators from the Texas A&M biomedical, industrial and systems, and computer science engineering departments, and one from Healthy South Texas, a Texas A&M outreach entity. “Only a multidisciplinary team could accomplish this broad spectrum of tasks,” said Coté. Additional co-principal investigators include Dr. Ricardo Gutierrez-Osuna, a computer science and engineering professor; Dr. Mark Lawley, department head of the industrial engineering department; and Starr Flores, the regional director of Healthy South Texas.
“We feel extremely proud, not only because access to research funds right now is limited, but most important, the societal value of this work,” said Sasangohar. “It’s concrete and impactful, and it puts us on the right path to revolutionizing diabetes technology.”