 A noninvasive device that enables doctors to quickly and accurately identify cancerous tissue in a person’s mouth is a step closer to reality thanks to an international collaboration between Texas A&M University and Qatar aimed at more effective diagnosis and treatment of oral cancer.
A noninvasive device that enables doctors to quickly and accurately identify cancerous tissue in a person’s mouth is a step closer to reality thanks to an international collaboration between Texas A&M University and Qatar aimed at more effective diagnosis and treatment of oral cancer.
The collaboration is supported by a three-year, $800,000 grant from the Qatar National Research Fund (QNRF) that will enable development and deployment of a handheld device for detecting oral cancer that will be tested at Rumailah Hospital, Hamad Medical Corporation (HMC) in Qatar, says Javier Jo, associate professor in Texas A&M’s Department of Biomedical Engineering. Jo, who is lead researcher on the project, is working with colleagues from Texas A&M at Qatar, Qatar University and HMC to develop the potentially life-saving tool that makes use of technology known as “fluorescence lifetime imaging (FLIM).”
Using FLIM, Jo explains, his team can measure and visualize the biochemical changes that occur in oral epithelial tissue as it turns cancerous. Measuring these specific changes, the technology, Jo says, can assist physicians in detecting and differentiating precancerous, cancerous and benign lesions in a patient’s mouth. Jo presented his research at last year’s World Molecular Imaging Congress, a venue where scientists and clinicians discuss cutting-edge advances in molecular imaging. His work with the Qatar team will focus on the continued refinement of the technology.
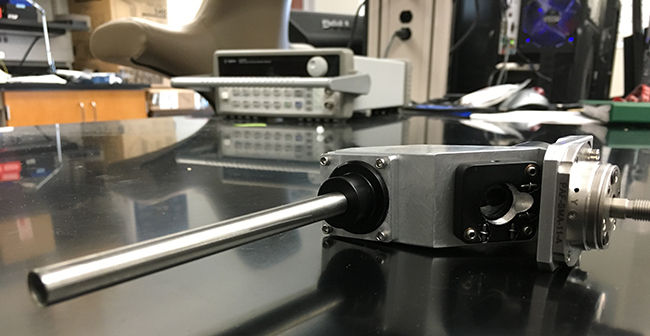
The primary goals of this phase of the project, Jo explains, are to scale down the device so that it is easier to use and increase the speed at which the device captures images from the oral cavity. In addition, the team is working to create and refine the algorithms needed to process the image information so that physicians can be provided with accurate information about the tissues they are examining in real time.
This type of instrument, Jo says, could make a significant impact at home and abroad. The National Institutes of Health estimates more than 8,000 people in the United States will die from oral cancer and another 37,000 new patients will be diagnosed this year alone. In Qatar, the disease is rapidly growing and could soon form up to a third of all cancer cases, according to the Qatar National Cancer Strategy.
“The successful completion of this research will result in a working prototype of a clinical tool for noninvasive real-time detection of epithelial precancerous and cancerous lesions in the oral cavity.”
Even more troubling, identification of oral cancer can be challenging, Jo says. Doctors typically rely on the naked eye to look for problematic areas in a patient’s mouth that warrant a biopsy, but identifying these areas can be difficult because a patient’s mouth can manifest lesions that may be both benign and precancerous/ cancerous, he explains. These different types of lesions are indistinguishable to the naked eye, and even some imaging tools experience difficulty distinguishing between them, resulting in false positives and triggering unnecessary and painful biopsies, Jo adds. Furthermore, tissue from a biopsy may register as benign, but the surrounding tissue that was not biopsied can be cancerous and remain undiagnosed.
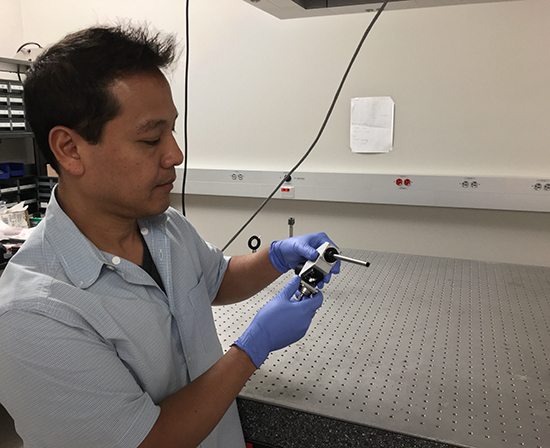
Jo’s device, which is essentially a small, handheld microscope, employs the FLIM technique to noninvasively evaluate tissue for the structural and molecular changes that serve as key indicators in determining if tissue is precancerous or cancerous. With the tool, Jo can observe distinct fluorescence signatures – molecular fingerprints of a sort – that are specific to benign, precancerous and cancerous tissue.
This enhanced identification is critical to early detection, Jo explains, but it also is an important tool during the surgical removal of cancerous tissue from a patient’s mouth. During surgery, physicians are tasked with the challenge of removing all cancerous tissue from the oral cavity while leaving intact as much surrounding healthy tissue as possible.
The current practice is to remove a 10 mm normal-looking border around the cancerous lesion, if anatomically possible, Jo says. However, the high rate of recurrence of carcinomas at the primary site indicates the inadequacy of this approach, he notes. In other words, trace amounts of cancerous tissue can get left behind, but Jo’s technology would provide surgeons instantaneous visual feedback about the tissues they are removing for a more directed, accurate extraction.
“The successful completion of this research will result in a working prototype of a clinical tool for noninvasive real-time detection of epithelial precancerous and cancerous lesions in the oral cavity,” Jo says. “Such a tool could potentially be used to assist at every step involved on the clinical management of oral cancer patients, from early screening and diagnosis, to treatment and monitoring of recurrence.”
The grant is made possible by the National Priorities Research Program (NPRP), the flagship funding program of QNRF. It is intended to foster a research culture in Qatar by encouraging the local population to embrace research and development. Grants awarded through the program are aimed at building human capital in Qatar; funding research to benefit the nation, the region and the world; and raising Qatar’s profile within the international research community.
Joining Jo in this research are Beena Ahmed, a signal processing expert from Texas A&M at Qatar; Nasir Rajpoot, an image analysis expert from Qatar University; and Zeynel Dogan and Hussain al-Enazi, senior otolaryngology surgeons at HMC.
About the Department of Biomedical Engineering
Committed to solving the world’s greatest health problems through the exploration of new ideas, integrated research and innovation, the Department of Biomedical Engineering at Texas A&M is producing the next generation of biomedical engineers, developing new technologies and new jobs, and achieving revolutionary advancements for the future of health care. The department has unique strengths in regenerative engineering, medical augmentation, molecular diagnostics/theranostics, tele-health, and precision medicine, and its faculty members are internationally recognized with collaborative relationships that span engineering, physical and natural sciences, medicine and veterinary sciences.
Contact: Javier Jo, associate professor in the Department of Biomedical Engineering at Texas A&M at 979.458.3335 or via email: javierjo@tamu.edu or Ryan A. Garcia, communications manager at 979.847.5833 or via email: ryan.garcia99@tamu.edu.