 A new synthetic material that’s strong enough to fill gaps in bone while stimulating new bone growth could advance the grafting treatments needed by people suffering from bone cancer and other bone defects, says a biomedical engineer at Texas A&M University who is developing the technology.
A new synthetic material that’s strong enough to fill gaps in bone while stimulating new bone growth could advance the grafting treatments needed by people suffering from bone cancer and other bone defects, says a biomedical engineer at Texas A&M University who is developing the technology.
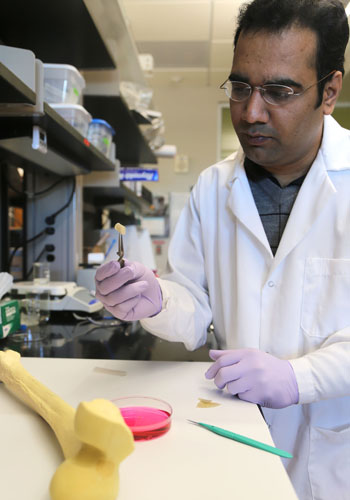
The material serves as a biodegradable scaffold that can be surgically implanted within the body to promote healing by triggering bone regeneration at the cellular level, says Akhilesh Gaharwar, assistant professor of biomedical engineering at Texas A&M. His research is detailed in the scientific journal Acta Biomaterialia.
With more than two million bone-grafting operations occurring worldwide each year, bone is the second-most transplanted organ, following blood, Gaharwar notes, but existing procedures can be limited by the amount of viable bone a patient can surrender. Some synthetic replacements are available, he adds, but they can cause side effects, be outright rejected by the body or become brittle and break under the loads they experience. In addition they can be difficult to cut and shape to fit a bone defect, particularly in instances where pieces of bone are removed to facilitate the extraction of a bone tumor, he says.
Looking to overcome these obstacles, Gaharwar, who was named a 2015 Young Innovator of Cellular and Molecular Bioengineering by the Biomedical Engineering Society, created a biomaterial that is strong yet flexible – think tire rubber – and that has the ability to boost the healing process by essentially telling pre-osteoblast cells (those cells in the body responsible for forming bone) to begin the regeneration process.
For Gaharwar, the work is an extension of his previous research developing an injectable material aimed at inducing bone formation for hard-to-heal bone fractures. This new material, however, is significantly harder and can absorb a greater load, he says, noting that it is intended for surgical implantation rather than injection.
Gaharwar’s material is made from embedding incredibly small particles of minerals called nanosilicates into a substance known as polyglycerol sebacate (PGS). Because PGS contains components already present in the body, it is rarely rejected and doesn’t cause side effects when it degrades, Gaharwar notes. Those properties, he says, make PGS a widely used material for a number of biomedical applications, but for bone engineering PGS needed to be stronger and interactive – in terms of “talking” to bone cells to initiate bone formation.
That’s where the tiny particles make a big difference.
So small that they are actually referred to as two-dimensional materials, these ultrathin nanosilicates have a high surface area but a thickness of a few nanometers or less. Think of a sheet of paper but on a much smaller scale. For example, a sheet of paper is 100,000 nanometers thick; Gaharwar’s nanosilicates are one nanometer thick and they contain orthosilicic acid, magnesium and lithium – minerals that induce bone formation.
By embedding these nanosilicates in PGS, Gaharwar was able to enhance the mechanical stiffness of the material by four times without affecting its elasticity. This allows the material the strength to sustain force while not breaking, he explains. In addition, the nanosilicates, once in place, signal bone cells to increase production of bone tissue. Early tests have demonstrated a 300 percent increase in alkaline phosphatase activity, a marker for early bone formation, and a six-fold increase in the presence of calcium phosphate, a main component of bone, Gaharwar notes. This is achieved, he says, without the use of proteins known as growth factors, which are used in conventional bone therapy treatments but can lead to serious side effects due to the large amounts required to stimulate cells.

What’s more, Gaharwar can control the rate of degradation for his material so that it works like a true scaffold, giving support when necessary and removing itself through natural degradation at the same rate as bone tissue is formed. Other commercial technology often fails when it degrades, leaving behind gaps, breaks and unsupported bone, Gaharwar notes.
Given these properties, Gaharwar believes his material can significantly help in bone regeneration for patients suffering from trauma, infection, congenital anomalies and oncologic resection.
“The addition of nanosilicates to PGS matrix significantly enhances the mechanical stiffness without affecting the elastomeric properties,” Gaharwar says. “The increase in mechanical stiffness and in vitro stability is mainly attributed to enhanced interactions between nanosilicates and PGS.”
About the Department of Biomedical Engineering
Committed to solving the world’s greatest health problems through the exploration of new ideas, integrated research and innovation, the Department of Biomedical Engineering at Texas A&M is producing the next generation of biomedical engineers, developing new technologies and new jobs, and achieving revolutionary advancements for the future of health care. The department has unique strengths in regenerative engineering, medical augmentation, molecular diagnostics/theranostics, tele-health, and precision medicine, and its faculty members are internationally recognized with collaborative relationships that span engineering, physical and natural sciences, medicine and veterinary sciences.
-30-
Contact: Akhilesh Gaharwar, assistant professor in the Department of Biomedical Engineering at Texas A&M University, at (979) 458-5540 or via email: gaharwar@tamu.edu or Ryan A. Garcia at (979) 847-5833 or via email: ryan.garcia99@tamu.edu.