New technology that transforms a cell phone into a powerful, mobile microscope could significantly improve malaria diagnoses and treatment in developing countries that often lack the resources to address the life-threatening disease, says a Texas A&M University biomedical engineer who has created the tool.
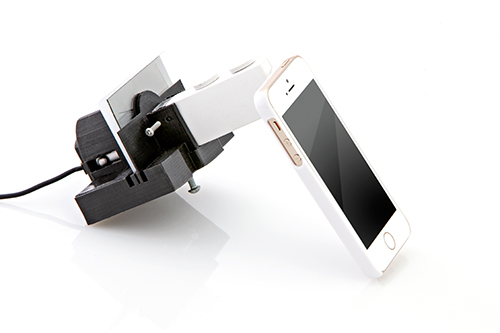
The add-on device, which is similar in look and feel to a protective phone case, makes use of a smart phone’s camera features to produce high-resolution images of objects 10 times smaller than the thickness of a human hair, says Gerard Coté, professor of biomedical engineering and director of the Texas A&M Engineering Experiment Station’s Center for Remote Health Technologies and Systems. Coté’s development of the instrument, known as a mobile-optical-polarization imaging device (MOPID), is detailed in the online scientific journal Scientific Reports, published by Nature. The full article can be accessed at www.nature.com/articles/srep13368.
MOPID, Coté explains, is capable of accepting a small cartridge containing a patient’s blood-smear sample. The sample is then imaged using polarized light in order to detect the presence of hemozoin crystals, Coté notes. Hemozoin crystals are the byproduct of the malaria parasite, and they occur in the blood of an infected host. As polarized light bounces off of these crystals, they appear as tiny bright dots when observed through the phone’s camera lens – enabling an instant, accurate diagnosis.
While polarized light has been the preferred option for malaria detection due to its increased sensitivity, its implementation into mainstream microscopy has been hindered by its complex configurations, maintenance, size and cost – up until now.
“What we’ve achieved with MOPID is the design of a polarized microscope platform using a cell phone, which can detect birefringence in histological specimens infected with the malaria parasite,” Coté says. “It’s a simple, low-cost, portable device that we believe is more sensitive than the standard rapid diagnostic tests (RDTs) and potentially as accurate as standard microscopy or the more complex polarized microscope.”
MOPID could represent a significant advancement in the detection methods for malaria, a disease that the World Health Organization estimates was responsible for 584,000 deaths in 2013, along with an estimated 198 million new cases in that span of time. Given those numbers, a dire need exists for a low-cost, accurate and portable method of detection, particularly in areas of the world with few resources, Coté says. Many of these regions, he notes, suffer from misdiagnoses due to inadequate or even nonexistent medical infrastructures – and the consequences can be devastating. While failure to treat malaria can be fatal, the administering of unnecessary malaria medications as a result of misdiagnoses can results in new, drug-resistant strains of the disease in addition to increasing costs for malaria medications, Coté notes.
Coté’s solution takes advantage of existing mobile phone technology and networks – something to which a whopping 75 percent of the world has access. This ever-increasing access to mobile networks and the fact that most mobile phones are equipped with advanced camera features make mobile phones the ideal platform for advanced imaging applications such as MOPID, Coté says.
The MOPID system has demonstrated both the resolution and specificity to detect malaria with both iOS- and Android-based devices and requires less user expertise than traditional microscopy, Coté says. That user-friendly aspect, coupled with the system’s portability and expected low cost of about $10 per unit, makes it an easily adoptable technology in low-resource areas ravaged by malaria, he adds.
What’s more, analysis of a blood sample can be instantaneously made with the patient in the field without the need for a mobile network, says Coté, who notes that a network is only required for transmitting the images to a central location for further analysis or storage.
“These factors increase the likelihood of adoption of the technique in developing countries where cost, complexity and lack of expertly trained technicians can often prohibit the use of a polarized microscopy technique or even traditional laboratory microscopy as the standard of diagnosis,” Coté says.
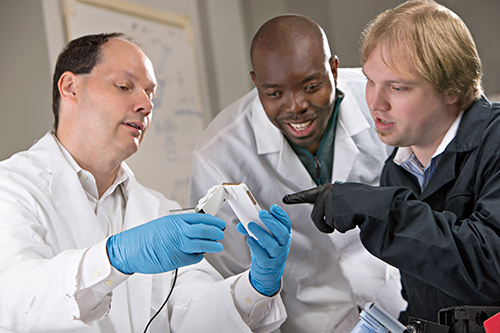
For now, Coté and graduate student Casey Pirnstill are continuing to refine the design of the system by making it more compact as well as improving its durability. Plans for in vivo field-testing are scheduled to take place in Rwanda, Africa in the near future, Coté notes.
About the Center for Remote Health Technologies and Systems (CRHTS)
The Center for Remote Health Technologies and Systems is designing and developing advanced health technologies and systems to enable healthy living through health monitoring and disease diagnosis, management and prevention. The center’s mission is to identify and overcome the unmet needs of patients and health care providers through the development of breakthrough remote health care devices, biosignal mapping algorithms, remote health analytics and information systems that will improve access, enhance quality, and reduce the cost of health care.
About the Texas A&M Engineering Experiment Station (TEES)
As an engineering research agency of Texas, TEES performs quality research driven by world problems; strengthens and expands the state’s workforce through educational partnerships and training; and develops and transfers technology to industry. TEES partners with academic institutions, governmental agencies, industries and communities to solve problems to help improve the quality of life, promote economic development and enhance educational systems. TEES, a member of the Texas A&M University System is in its 100th year of engineering solutions.
Contact: Gerard L. Coté, professor in the Department of Biomedical Engineering and director of the Center for Remote Health Technologies and Systems at 979.845.4196 or via email: gcote@tamu.edu or Ryan A. Garcia at 979.847.5833 or via email: ryan.garcia99@tamu.edu.